What is breast density and why is it important?
What is breast density?
You might be surprised to know that breast density doesn’t have anything to do with size, and that it’s one of the first things breast imaging professionals will analyse. We’re going to break down exactly what breast density is, how it can change over your lifetime, and its importance in clinical imaging.
Dense breasts must be big breasts, right?
Not quite - contrary to popular belief, breast size isn’t an indicator of density1, because density refers to how much of the breast is made up of glandular tissue (the tissues that produce and store milk) versus fat. If you need a recap on the tissue types in a breast, check out our breast anatomy breakdown here.
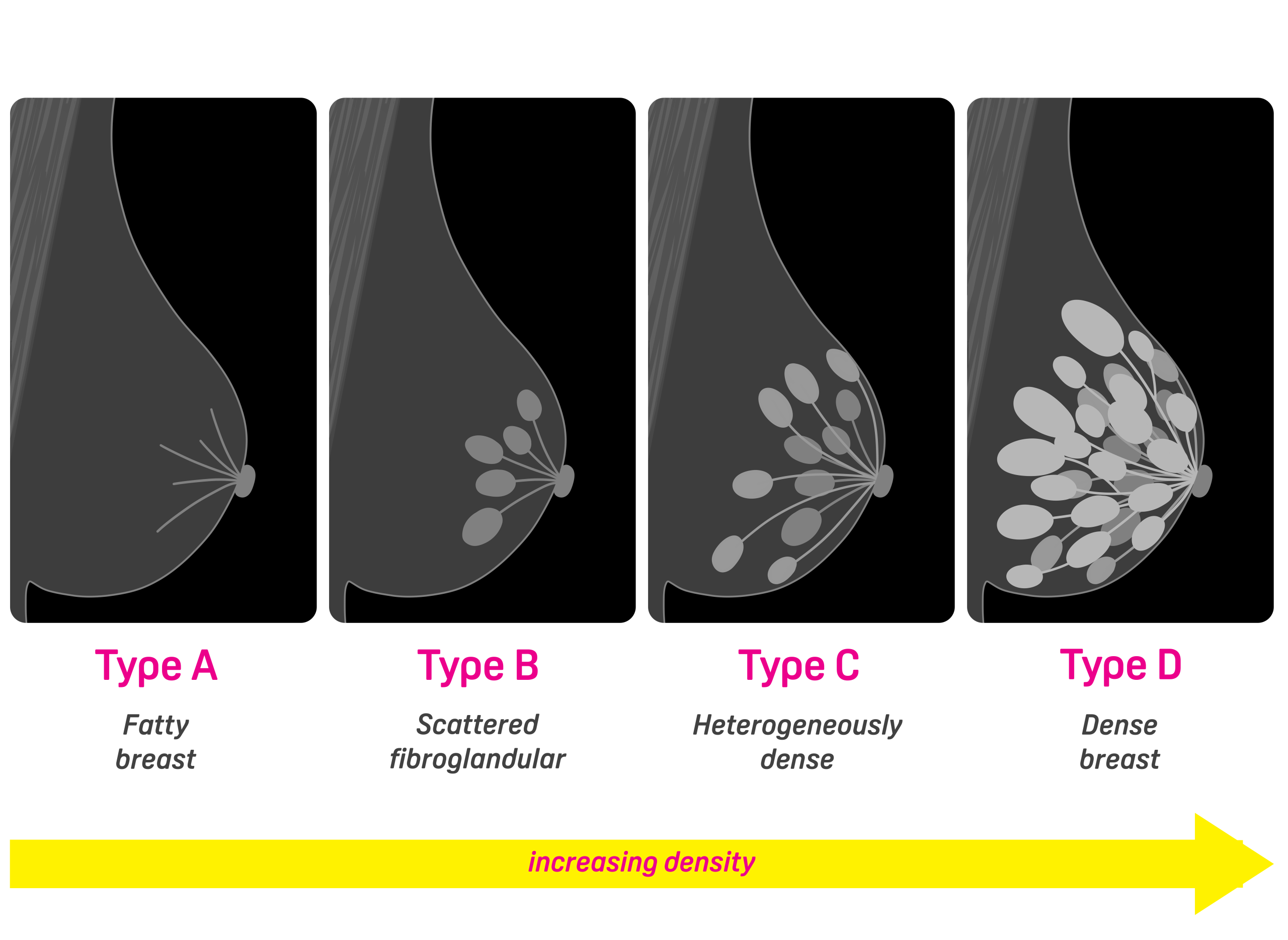
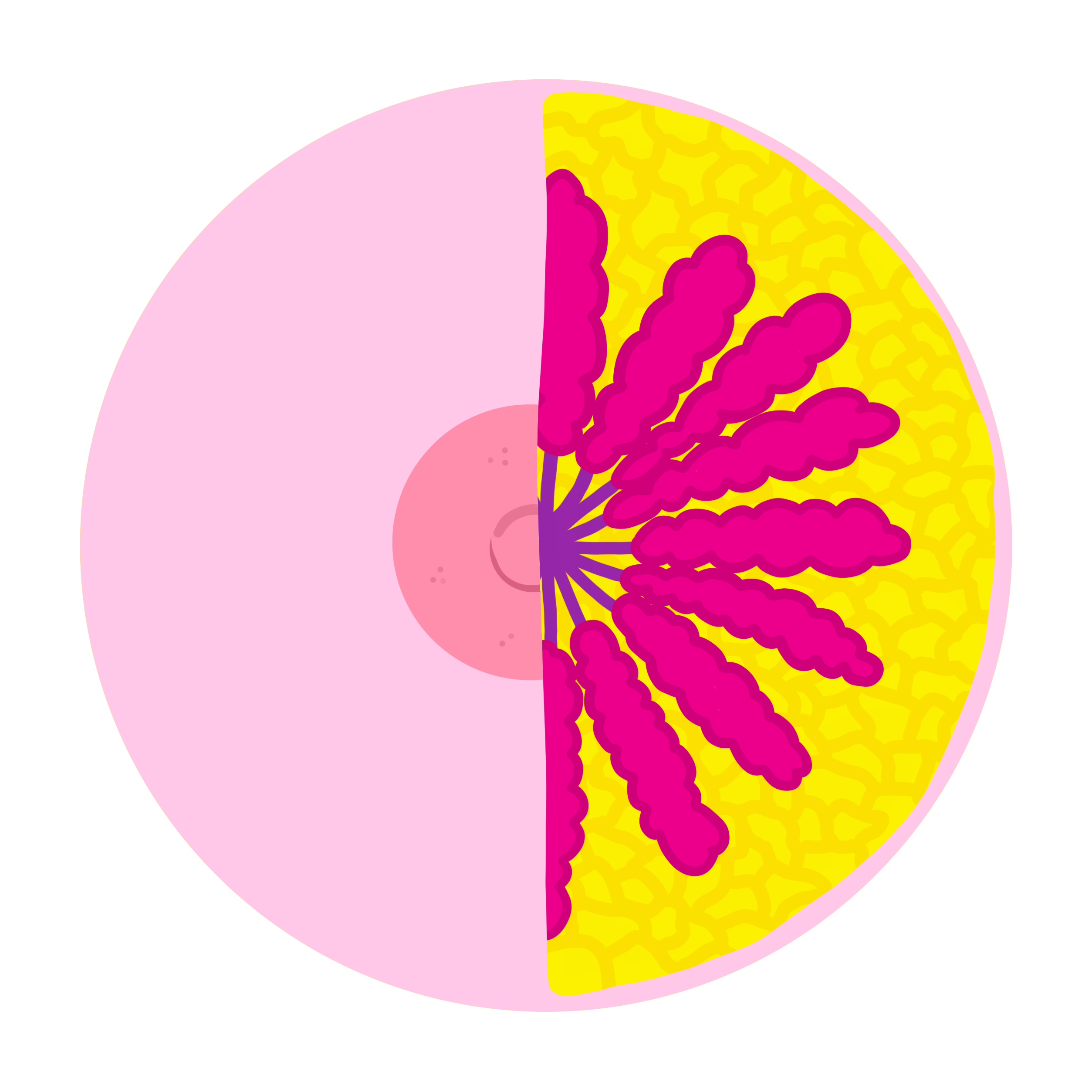
As you can see above, the more of that glandular tissue (the lobes and the ducts) that is present, the denser the breast – this is what that actually looks like under mammography, where the leftmost image is a fatty breast and the rightmost image is a dense breast:

What determines your breast density?
Your breast density is largely down to your genetics, although age, exercise and overall body fat percentage can impact it.
Some studies have shown that breast density may be higher in women who started their period at a later age, had children later in life, or are undergoing hormone therapy (HT)2.
How does breast density
change over time?
When you are young, you are more likely to have dense breasts. It makes sense when you think about it – if we know that breast density is about how much glandular (milk-producing) tissues there are in the breast, this is going to be higher while you are of reproductive age. As we get older, the breasts become less dense - most notably during menopause - as the glandular tissues breaks down.
Why is breast density clinically important?
To make sense of why breast density is clinically important we need a basic understanding of X-rays, because mammography (the main imaging modality used for breast screening and assessment) is a type of X-ray.
When you think of an X-ray, you probably think of the skeleton – bones show up white in an X-ray because they are dense and absorb more of the X-rays. Less dense tissues absorb less radiation, so muscle, fat and soft tissues appear darker. Because glandular tissue is dense, it appears much brighter than fat.
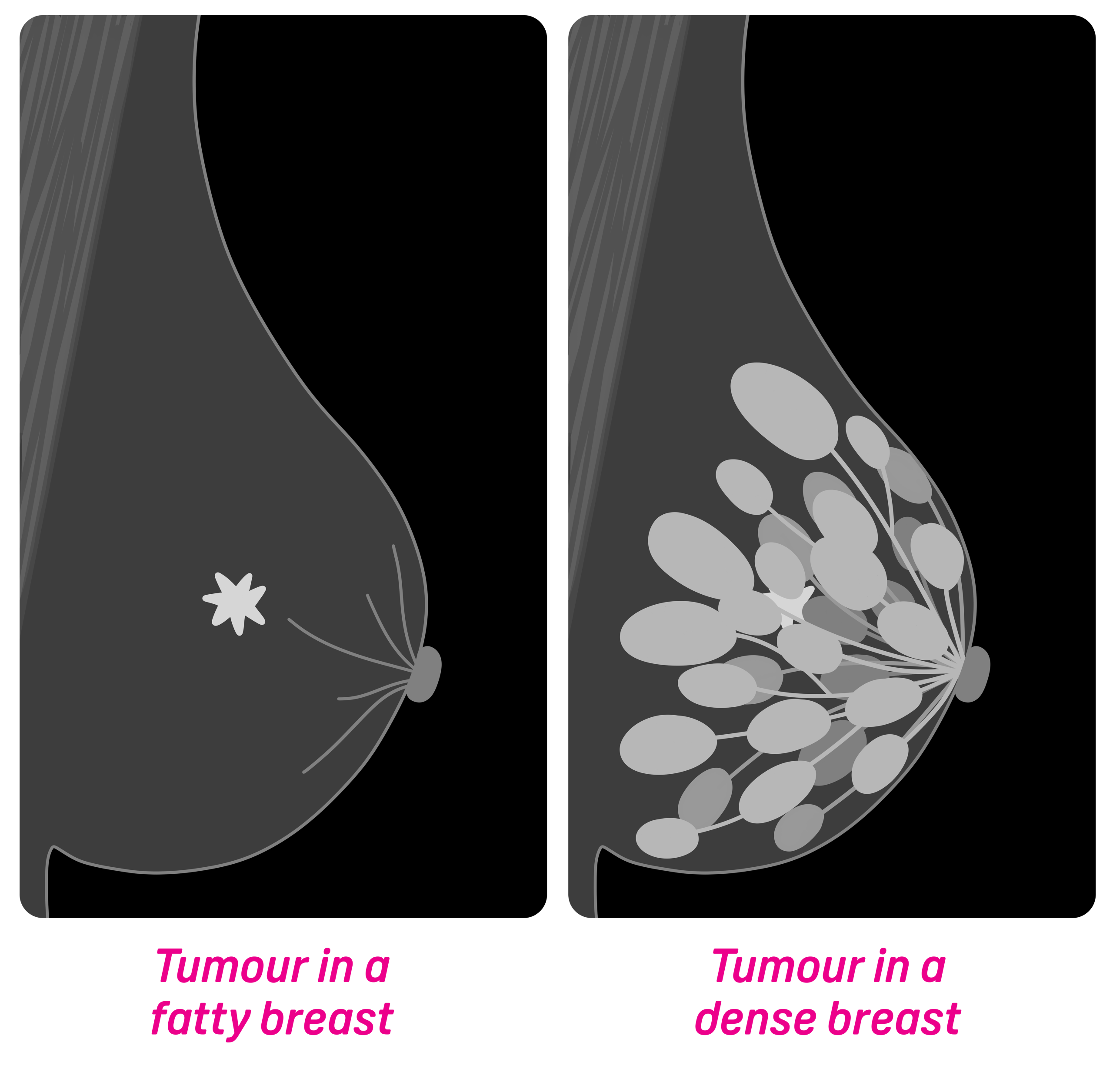
This is important because it can make breast cancers more challenging to spot in a dense breast due to the low contrast with the surrounding tissue. Take the below example; there is a tumour in both of these breasts, but which one is easier to spot?
How do clinicians overcome
these challenges?
Tomosynthesis
Often referred to as just ‘tomo’, tomosynthesis is when multiple X-ray ‘slices’ are captured of the breast, so that the tissue can be examined in more detail on multiple planes of the breast. As opposed to one flat image, the clinicians can scroll through several layers of images to make sure nothing is being masked by dense tissue. A lot of breast clinics in the UK now have tomosynthesis built into their mammography equipment.
CEM
There is also a technique called Contrast Enhanced Mammography (CEM), which combines the use of a contrast medium with traditional mammography. The injected contrast flows through the vascular structures (blood vessels of the breast), highlighting any abnormalities. This works really well because cancers are greedy – they require a lot of blood to grow, so there are often more blood vessels or leaky blood vessels around the site of a tumour.
MRI
MRI is a great option for imaging dense breasts too. It works totally differently to mammography, so dense tissues aren’t a problem. It is really sensitive too, so even tiny cancers are easier to detect.
Ultrasound
Ultrasound can be another good option, particularly if a patient presents with a palpable lump. It is one of the most widely used imaging modalities, and is readily available in a lot of departments.
Can I request a different imaging modality to
2D mammography for screening?
All screening is conducted using traditional mammography, and you cannot specifically request a certain modality. If, hypothetically, you attended screening and your breasts were so dense that your scans couldn’t properly be evaluated, you would most likely be recalled for further imaging. Breast imaging professionals are incredibly thorough, and each scan is evaluated by two different clinicians to minimise the chances of anything being missed.
Are people with dense breasts at higher risk of breast cancer?
It isn’t a straightforward answer, but ultimately the more glandular tissue in your breast, the more at risk you are of developing breast cancer. This is because breast cancer usually starts in the ducts or the lobes.
A study by the Breast Cancer Detection Demonstration Project (BCDDP) found that women who had a breast density score of 75% or greater (BIRAD D) at the time of their first mammogram had an almost five-fold increased risk of breast cancer compared with women who had no visible dense tissue3.
How can I find out my breast density?
Breast density cannot accurately be determined by feel or touch and does not correlate with breast size4. Until you have a mammogram or another type of imaging at either a screening or assessment clinic, you can’t really find out your breast density. It won’t impact your health or day-to-day activities – it’s only important for breast clinicians to identify breast density to make sure the care that they receive is what is best for the patient. While it is standard practice in the USA to tell patients if they have dense breasts, this is not the case on this side of the pond.
In the UK, women are invited to attend breast screening every three years between the ages of 50 and 70. It’s really important to get your mammograms when invited, because the key to beating breast cancer is early detection. If you want to know more about what happens at breast screening, you can check out our guide here.
References
- Baldwin, C. J., Albrecht, S., Lee, J. & Neergård, J. (2010) ‘The variation in breast density and its relationship to breast size’, Breast, 19(5), pp. 406–410. DOI
- Titus-Ernstoff, L., Tosteson, A. N. A., Kasales, C., Weiss, J., Goodrich, M., Hatch, E. E. & Carney, P. A. (2006) ‘Breast cancer risk factors in relation to breast density (United States)’, Cancer Causes & Control, 17(10), pp. 1281–1290. doi:10.1007/s10552-006-0071-1.
- Cancer.gov. (2025). Breast Density Research in DCEG. [online] Available at: https://dceg.cancer.gov/research/cancer-types/breast-cancer/breast-density.
- Vukasin, F. (2023) ‘Breast density: Should it be reported?’, newsGP (RACGP), 31 March. Available at: https://www1.racgp.org.au/newsgp/clinical/breast-density-should-it-be-reported?



